Medicaid Expansion Could Have Prevented 745 COVID-19 Deaths in North Carolina
The COVID-19 pandemic has given North Carolina one more reason to join the 38 other states that have received federal dollars for Medicaid expansion. Given that the United States is the only industrialized country without nationalized health care (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1447684/ ) has the highest total death count of any country (https://www.statista.com/statistics/1093256/novel-coronavirus-2019ncov-deaths-worldwide-by-country/) and the fifth highest per capita death rate in the world (https://coronavirus.jhu.edu/data/mortality), we sought out to see if there was any evidence to suggest a correlation between uninsured rates and COVID-19 deaths.
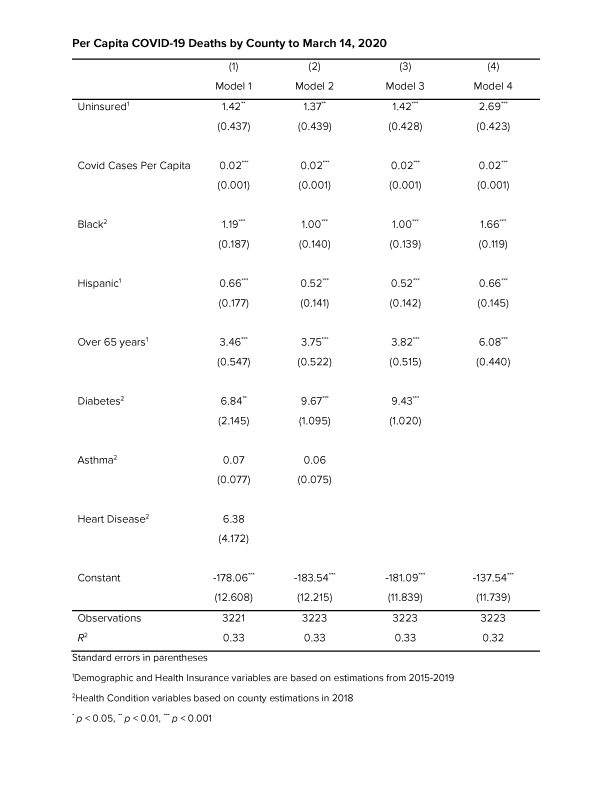
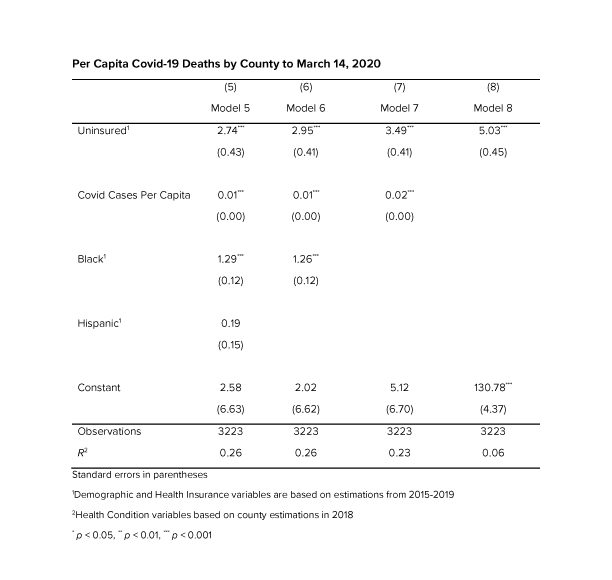
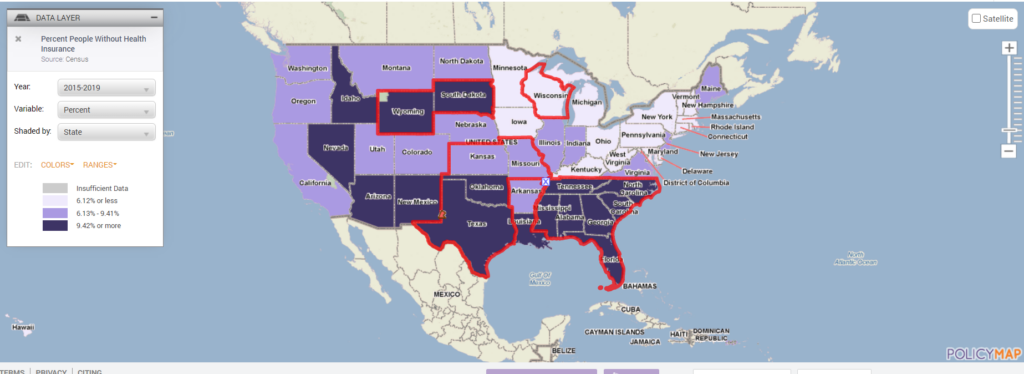
Studies show that people without insurance report delaying or simply foregoing necessary medical treatment due to cost (https://www.kff.org/report-section/the-uninsured-and-the-aca-a-primer-key-facts-about-health-insurance-and-the-uninsured-amidst-changes-to-the-affordable-care-act-how-does-lack-of-insurance-affect-access-to-care/). We hypothesized that counties with a population that have higher percentages of uninsured would have higher rates of COVID-19 deaths when controlling for per capita COVID case rates. County wide data for all 50 states and Washington DC was downloaded from Policymap.com, which aggregates data from a number of sources including the Census and data from the New York Times COVID Tracking Project, To create a more robust dataset we also controlled for percentage of those aged 65 plus as well as the percentage of black and Hispanic populations, due to data which suggests that the death rates among blacks and Hispanics is higher than the percentage of blacks and Hispanics among the total U.S. population. (https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html) We also added underlying health conditions correlated to higher COVID-19 morbidity to the model based on Census data which estimated the percentage of the population with the conditions.

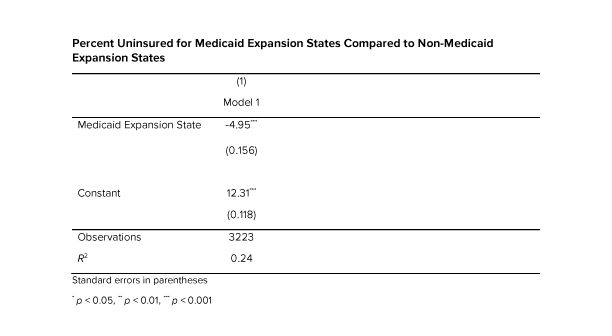
The model showed that with all the variables being held equal for every one percent increase in uninsured rates an average 1.4 more people will die of COVID per 100,000, which is statistically significant at the 1% level. In 2019, North Carolina had the 9th highest uninsured rate in the U.S. of 11.4% compared to the national average of 9.2% (https://www.kff.org/other/state-indicator/total-population/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Uninsured%22,%22sort%22:%22desc%22%7D). According to the dataset Medicaid expansion states have uninsured rates an average 4.95% lower than non-Medicaid expansion states, which is statistically significant at the .001 level. This falls right in line with the estimated 400,000-620,000 people currently in North Carolina’s coverage gap who could benefit from Medicaid expansion and represents 3.8-5.9% of North Carolina’s population (https://www.ncchca.org/community-resources/policy-advocacy/nc-insurance-gap/ ) If North Carolina was a Medicaid expansion state our uninsured rate would be about 5% lower than it is now. According to our model 5 percent lower uninsured rate would have resulted in an average of 7.1 fewer COVID-19 deaths per 100,000, which extrapolated to North Carolina’s population of 10.49 million means that expanding Medicaid could have saved the lives of close to 745 North Carolinians.